Questions I asked
December 26th, 2023
1. Is the risk of STDs higher, lower or the same after surgery?
about the same
2. Is the risk of a vaginal infection similar to a cis womans? From a google search there’s around a 3-4 pH difference between peritoneal fluid and vaginal fluid. This would result in different microbe colonization, is that something I’d have to look out for or preempt?
bacterial vaginitis risks are similar; peritoneal fluid has neutral pH (about 7.4) and cervical fluid is lower; this changes the biome and makes staph infections more common after this operation
3. I’m assuming I might have to take a low dose of testosterone post-surgery given I won’t have testes or ovaries. I know it’s produced in other regions of the body as well, but what have your patients experienced? My current plan is to have more regular hormones tests after surgery, cease testosterone blockers and adjust accordingly.
testosterone goes up after surgery (as the blockers stop >99% of your bodies testosterone from working, and after the op, 10% of your testosterone production continues from the adrenal gland but is no longer blocked)_; my experience is minimal patients have testosterone replacement - this is guided by endocrinologists
4. I’m assuming I’ll need a gynecologist after this right?
it is useful
5. Should I expect any physiological/physical changes post-surgery? (unrelated to the actual surgery) I’d assume not, since I’ve already been on hormones for multiple years, but I’m not sure how still having testes would be influencing my current body.
unrelated to surgery, some people do find they might change their oestrogen regimen, again I leave this to the endocrinologist and GPs
6. Are there any items you’d recommend me to have after that first week in hospital? I imagine it’ll be quite an ordeal. Currently I’m just looking at a donut cushion, but I’m interested in anything else you think would be good to have.
donut cushion is number 1
salt baths are number 2
lube is number 3
in time some patients use different dilators, but that doesn’t tend to be an issue until about week 6 post-op
Jan 10th, 2024 - Surgery
Jan 18th, 2024
How far should the purple dilator go? At the moment I am reaching the last of the 3 white dots.
that depth is fine - it will vary a few cm here and there as things heal and the swelling settles. I’d make a point of knowing where the dilator is now and then weekly assess what the depth is
I’m scared of pushing the back of the vagina and hurting it, how do I tell what is far enough depth when dilating?
with gentle pressure (so not painful) the dilator won’t go any further in
The parts below the opening look really scary, is it normal for them to look like that? and what’s with that weird lump looking thing by the stitches on one of the labia(not sure if it’s part of the labia)?
very normal - this is the area with most tension. Sometimes it splits a little. salt baths help this area heal. there is often some. the bump looks like some bullous inflammation (sometimes the skin’s reaction to dressings, sutures or healing)
I accidentally moved my leg to the side when I was on the toilet and made something lower down bleed, it wasn’t a significant amount of blood mostly watery brown on the pad but it worried me
you’ll get blood intermittently with dilating. this small amount is ok but let me know if you are worried
why is this one wound on my stomach like this? it’s pieced itself together poorly without a steri strip over it and I’m worried it’ll leave a bigger scar than it has to, how do I fix it? it has two risen bits of flesh that are displaced vertically from one another, why didn’t someone just cover it properly with another strip?
the skin doesn’t like to heal in a vertical fashion (like this scar), unfortunately that’s the only way to get the camera in for the operation. It is only 8 days after the incision. It will heal in time
also do you know any gps or anyone that I could see in the remaining 6 days I’m here? it’s in your discharge papers as something to have done but there was nothing in the pretext for this operation so every gp in Canberra is booked out it seems, it’d be a good idea to tell interstate patients this so we could book appointments prior.
it is more of a generalized comment to see probably your GP in a week or two. The 25th in [city] is completely fine.
I have an appointment back in [city] on the 25th, but it worries me that (as someone with limited medical knowledge) im going to be the only one to check on it physically during this time. I know I can send you photos but it still worries me.
just email me any issues. it is all healing up fine. most of the time patients just need reassurance, and at present all your wounds are healing as expected.
Jan 22, 2024
What’s the schedule with dilating for the future? 3x per day for the first few months, what about after that?
yep - 3x day for 4-6 weeks
then 2x/day for a month or so
daily for about 6 months and then 1-2 weekly forever.
Jan 27, 2024
the stitch itself is this one singular bit now, I remember sending you a photo of a bulbous bit of healing previously and it’s that same stitch. I think part of its broken off on that side, should I just cut off this other loose bit? or pull it through? not sure what to do
you can cut it loose flush with the skin
all the sutures have served their purpose - the tissue is now holding everything together
Feb 5th, 2024
An update and a few questions,
I’m currently dilating 3x per day, all going well. I got a set of soul source GRS dilators and I’m comfortably using the 1-1/8” one (working on 1-1/4”) with about 13ish cms of depth, is this all pretty typical around the 3.5 week mark?
I took out the stitches that I could reach like you said, all went fine and walking is much more comfortable now. The irritation that stich was causing is all gone, and everything overall looks like to be healing well : )
I stopped having blood in my discharge around the 25th (15 days post op) and pretty much no discharge since. Currently, when I dilate, I get some very pungent yellow “slough” (what the internet told me it was) coming out, it basically looks like yellow snot. I’m guessing it’s a mix of dead cells, lube, and stitches dissolving (if there’s stitches up there idk). It does not smell great, but I don’t expect a healing area to smell great anyway- it’s kinda like a garbage smell without the nastiness, or very stinky socks. I haven’t ever smelt anything like it before honestly, I can only smell it when I dilate (and even then I have to get close to the goop to smell it) and there’s no odour usually. I guess I’m just disturbing all that mess when I dilate? I have a shower after I dilate and then it’s all fine, I just use soapy water around the outside and use a finger to get rid of any remaining stuff inside.
regarding the discharge and smell - they are all “normal” and exactly as described. Try some salty water or lavendar soap douching as this gets the slough out of there and helps reduce the bacterial load (which is what smells).
Other questions:
· Should I be trying to establish certain types of bacteria? I’ve seen people online talking about vaginal probiotics for this purpose. I don’t imagine you could officially recommend anything that isn’t proven to work for liability or whatever, but if you’ve had any anecdotal evidence from your other patients, I would appreciate it.
vaginal probiotics - not much evidence. I think so long as the area is not being sterilised so as to allow normal bacteria to proliferate should be adequate
· Are you the doctor to be asking questions about the vaginal microbiomes? Or would you prefer I ask these questions to a gynaecologist with some neovagina experience?
me or the gynae regarding vaginal microbiomes. Although as said, there’s not a lot of evidence to help it along with pro-biotics.
· Does the kind of lube matter beyond water based, e.g. the one I have has methyl hydrobenzoate (methyl paraben) as a preservative (Lubri-gel), will using something with an antimicrobial agent 3x per day affect whatever’s going on in there? I don’t want to be killing off any and every bacteria that’s tryna grow in there and risk an infection later on. If this matters, are there any particular lubes you’d recommend?
water based just tends to be gentler on the vaginal flora, and easier to clean/douche out; also is a neutral pH
· Since my pH is going to be around 7 from the peritoneal secretions, If i use anything lower than that would I risk messing up whatevers going on in there? For instance a lot of lubes are balanced around a cis vaginas pH, I’m struggling to find much information about this and other PPV things online.
· What level of lubrication/secretions I should be expecting with PPV? Should it be enough to not worry about douching unlike other surgeries?
levels of discharge - variable for 12 months, and can be yellow/bloody/grey/white/clear/brown
· I’m getting a bit of bloody slimy looking stuff coming out the clitoral/urethral area, I’m assuming this is the “gunky stuff” you were talking about?
· Your discharge sheet says dilating for 3x daily for 15 minutes, that conflicts with what you told me, I’m assuming the sheet is wrong.
the discharge instructions that I emailed are the ones you should follow. The hospital has some weird old set that gets handed out variably to patients. I wouldn’t pay much attention to it. I’ve told them a million times to get rid of it, but every so often it pops up. To be honest though - no one in the world has the same dilating regime, so 15mins is probably ok, so long as it is not too painful. But I’d prefer 45mins
· My heart rate is quite high at the moment (100+ walking around) and has been since surgery, I’m walking as much as I feel capable of, is this normal? I stopped taking my ADHD medication once I left the hospital because of this and other reasons, but it doesn’t seem to have been the cause.
regarding heart rate - probably worth mentioning to your GP
· What’s the deal with only using the perineal raphe up one side of the vagina? It’s a very distinct cosmetic difference, I’m assuming there’s a reason why that lumpy weird bit couldn’t have been minimised or removed?
perineal raphe - are you talking about the midline raphe? surprisingly in everyone it isn’t actually midline once you hit adult hood (due to difference in scrotal growth velocity). The idea is to make the perineum as lax as possible (as this is where most revisions occur) and almost invariably the raphe ends up on the left or right and never on the midline otherwise the perineum becomes too tight (making dilating difficult, and requiring further operations). Over time, I haven’t had anyone have an issue with it. But just keep an eye on it for the time being
· Is there anything else I could be doing at the moment to improve my outcomes beyond what we’ve communicated in emails?
Just keep it simple - slowly get back into more activity, keep the dilating up, try pelvic floor exercises.
· I have a gp appointment on the first of next month, is there anything in particular I should let them know to look for?
GP - get them to have a look at the sutures more than anything else
Feb 7th, 2024
I noticed this hole appeared yesterday. I think it was caused by a stitch working its way out, I noticed a long thread so I pulled it out (it came out easily and didn’t hurt). Guessing that’s what caused this.
I attached a photo from last night and this morning. Is this anything I should worry about? I’ve been doing more salt baths because I figured that’s what you’d suggest. Just worried cause it’s in the area where all that bacterial nastiness comes out.
all good - these are called stitch granulomas and removing the suture helps it heal. Salt baths are good for. Rarely that area will turn into a small granulation area. keep an eye on it, but nothing to worry about
Feb 17th, 2024
Was finally bold enough to move things around and I noticed this interesting looking tissue on both sides.
it’s granulation and probably suture granulation tissue specifically.
I also noticed I’m rather numb in that entire as well (not just the funky tissue but the surrounding clitoral area, skin etc.).
Are either of these things cause for any concern? or is it typical?
not a major cause for concern. sometimes it settles by itself. sometimes it can reduce urethral opening. I’d try some hydrozole on the area.
Feb 19th, 2024
When I see my GP what should I ask her to check regarding the granulation? Anything specific?
gp - just to keep an eye on it and maybe a script for avantin if the hydrozole is not cutting it
Hydrozole I’m assuming for the hydrocortisone in the mixture rather than the antifungal? Can I just get OTC hydrocortisone instead?
i don’t think there’s an OTC hydrocort by itself, often needs a prescription because of high strength
March 21st, 2024
I’ve noticed that my right labia minora is much larger than the left and is painful to the touch while the other isn’t. It feels like there’s something swollen under the surface following the length of it.
it could be excess spongiosal tissue. i’d still give it more time. usually try to wait up to 6 months to fully assess swelling and it’s implications. in the event that it is still present down the track and it is an issue we would need to excise the excess.
is it normal to still have pain & swelling 10 weeks out?
most pain settles at around the the 3 months mark, but some patients do get issues with pain/discomfort for 12 months.
March 31st, 2024
got this weird red fleshy bit coming out of underneath the right labia minoria (same side where I was having swelling and pain). what do you reckon? I can’t feel the red thing if I touch it if that means anything. It’s only connected on the one right side bit and not underneath.
thats a small piece of granulation. Sometimes the hydrozole cream can settle it, but once it starts forming a stalk like that it may need to be cauterised off (can be done with silver nitrate by the GP is they are happy). Any time from now would be fine for that.
April 24th, 2024
Just wondering if it’s normal to still have quite pungent discharge after 3 and a bit months? It’s yellow in colour and smells very strongly. It’s the kind of smell where I wouldn’t want anyone near it at all.
try some lavender soap in the douche
could get the GP to do a self-swab for bacterial/fungal analysis as well
I haven’t been able to find any information online regarding this specifically for PPV or otherwise. Regarding douching there seems to be a conflict between douching helping with odour but disrupting the microbiome and making it worse in future. Again, the limited information I’ve found is for PIV not PPV specifically.
Also in future if I were to use a lower pH lube (as a lot of those on the market are pH balanced for a cis vagina) would that be something I should avoid given it’s always going to go back to neutral because of the peritoneal lining secretions? I’m struggling for information as it seems my GP doesn’t know much about this.
regarding pH, it’s probably best to use neutral as lower or higher will likely disrupt the bacterial lining too much
I have patients that do take 3-12 months for odour to settle for numerous reasons (natural biome, ongoing healing, granulation). there isn’t a particular cause and my feeling is that genetics probably play a big part
June 30th, 2024
I’ve recently felt some pain in where I think the inguinal canal area is (not entirely sure) — it’s horizontal and up a bit from where the clitoris is. It happens if I touch the area lightly or stretch my lower abdomen at all. On a scale from 1 (poking yourself hard) to 10 (epidural wearing off after surgery) I’d give it a 5. Any idea of what this is or should I be worried at all? I think I was enjoying my girlfriend’s thigh too much, but it’s been a couple days and it’s still really sore :(
Probably just a pulled muscle, but might be worth checking with GP to make sure it’s not a hernia or something else
August 18th, 2024
I was wondering if there’s a time minimum for considering revision surgery or a maximum where you wouldn’t consider it anymore. Also, what is the general cost/wait time for revision surgery?
Depends on what needs revising. If it’s the urethra or annoying granulation tissue - from 3 months. If it’s vaginal issues, about 3-6 months. If it’s aesthetics, probably about 12 months.
November 18th, 2024
I’ve been having some bleeding the past few days. It’s been making my discharge pink in colour and I’m noticing a small amount at the tip of my dilator along with some little blood clots. it’s not painful, is this something to worry about? I’m 10 months out from surgery now.
Not really. Worthwhile seeing GP. I would try some steroid on the dilator a few times per week. Probably granulation. Let me know how it progresses.
February 6th, 2025
The bleeding is still happening, mainly when I dilate. Outside of dilation it is occasionally clean from blood (discharge occasionally appears pinkish) but it seems to always happen after dilating.
I’m fairly gentle during dilation and I’ve tried being more mindful of dilating slowly but the bleeding continues regardless. I also haven’t been able to ‘feel’ a source, nothing feels painful internally apart from the usual stretching discomfort.
I spoke to my GP about it, they didn’t have much idea of what to do and since then I’ve moved to Melbourne and I’ve yet to find another GP.
How should I proceed and how should I advise my next GP? (Since I doubt many would be up to date on this surgery).
Given it has been going on for quite a while now without a response to steroids, it would be worth having an internal exam under anaesthetic to burn off any potential causes (and rule out other issues).
There are a couple of urologists in Melbourne that could help, otherwise I am happy to sort it out up here.
February 10th, 2025
Which urologists would you recommend in melbourne?
What kind of wait time would it be to have you sort it? And what kind of cost would be involved?
Gideon Blecher in Melbourne.
Wait-time for me - basically whenever. I can do it next wednesday.
Cost - if you are still privately insured; nothing for me; anaesthetist might be a couple of hundred dollars.
Let me know and I will give you some potential dates
March 17th, 2025
I also wanted to ask if you’d be able to investigate some other issues alongside the unknown cause of the bleeding while I was in Canberra.
Issue 1.
I’ve been experiencing a painful dull ache under the right labia, extending down my right inner thigh that has been consistent for the majority of this year. My best guess at a cause is the ilioinguinal nerve being compressed, or something else of that nature. My left leg and left side of my vulva is completely pain free.
Symptoms:
- If I wear clothing that is any kind of constrictive (underwear with elastic, jeans, etc.) the pain happens. I’ve had to start wearing exclusively loose fitting things
- If i sit the wrong way or cross my legs it hurts
- The only way to alleviate it is to lay down with my leg in a certain position (rotated outwards to the right)
- I had this rarely before surgery but after it it has been a daily occurrence and is getting pretty unbearable, and its degrading my quality of life
Issue 1 – sounds neural/musculoskeletal. Probably worth seeing a physio first up. Obviously will have a look when you are asleep, but unlikely to be anything to find that is reversible from my end.
Issue 2.
If I get aroused or sit on the toilet for too long the erectile tissue under my right labia gets engorged, uncomfortable and hurts, its also noticeably larger than the left side and affects urination. I’m not sure how much of the pain is related to issue 1.
Issue 3.
Urine direction is angled up toward my stomach, this may be a result of the erectile tissue on the right side of that area.
Issue 2/3 – usually due to the same thing. I can realign the urethra and debulk some of the underlying spongy tissue. Only thing with this is you need to stay in hospital at least a night.
Issue 4.
There is a bulb of tissue at the end of my vaginal canal. It feels like a ball the size of the end of my finger.
Have you encountered these issues before and would you be able to help me with them? Please let me know how we can proceed.
Issue 4 – as with above, if I can see it I can excise it at the same time.
March 25th, 2025
Would it also be possible to do additional hair removal while I’m under? There’s a few that grow quite close to and then into the vaginal area. I can also work out doing it on my own terms if you think that would be better.
Hair-removal - I will burn whatever is nearby, but it will undoubtedly need some laser or electrolysis as the hair follicle is pretty resilient.
For the urethral revision part - I leave a catheter overnight. There are some sutures in this area that rarely bleed, but may cause a bit of swelling. It is unusual to have anything terrible with this revision, worst thing I’ve seen is a patient had pelvic floor spasms and couldn’t pass urine for a few days. It still sprays for a little while after due to the swelling, but the aim is to get the direction right and reduce the pressure required by the bladder.
May 7th, 2025 - Revision surgery
May 13th, 2025
1. When can I get the stitches removed? I’m assuming 3 weeks like you said last time.
- The sutures should just dissolve and fall out, but can be removed from about next week if they are a nuisance.
2. I feel like I’ve lost a bit of depth, I’m assuming that’s just swelling. I’m going easy with dilating because of the stitches as they’re causing me a bit of pain, I shouldn’t lose this permanently right? as everything is as you said pretty mature.
- Depth change probably due to inflammation. Shouldn’t really change given I haven’t changed anything in the vault, only the introitus.
3. I didn’t understand what you said was done completely, I attached a diagram of what I think you did just to check if I got it right or not.
- I can see that the urethral webbing was cut and stitched but there’s also stitches down around the vaginal opening, was this where that additional webbing you were talking about was?
- that “bulb of tissue” i mentioned that you said was also webbing(?) I’m assuming it was also corrected by cutting and stitching. So there’s stitches up around there too right?. Was this webbing what was causing the bleeding I was having somehow ? or was it granulation?
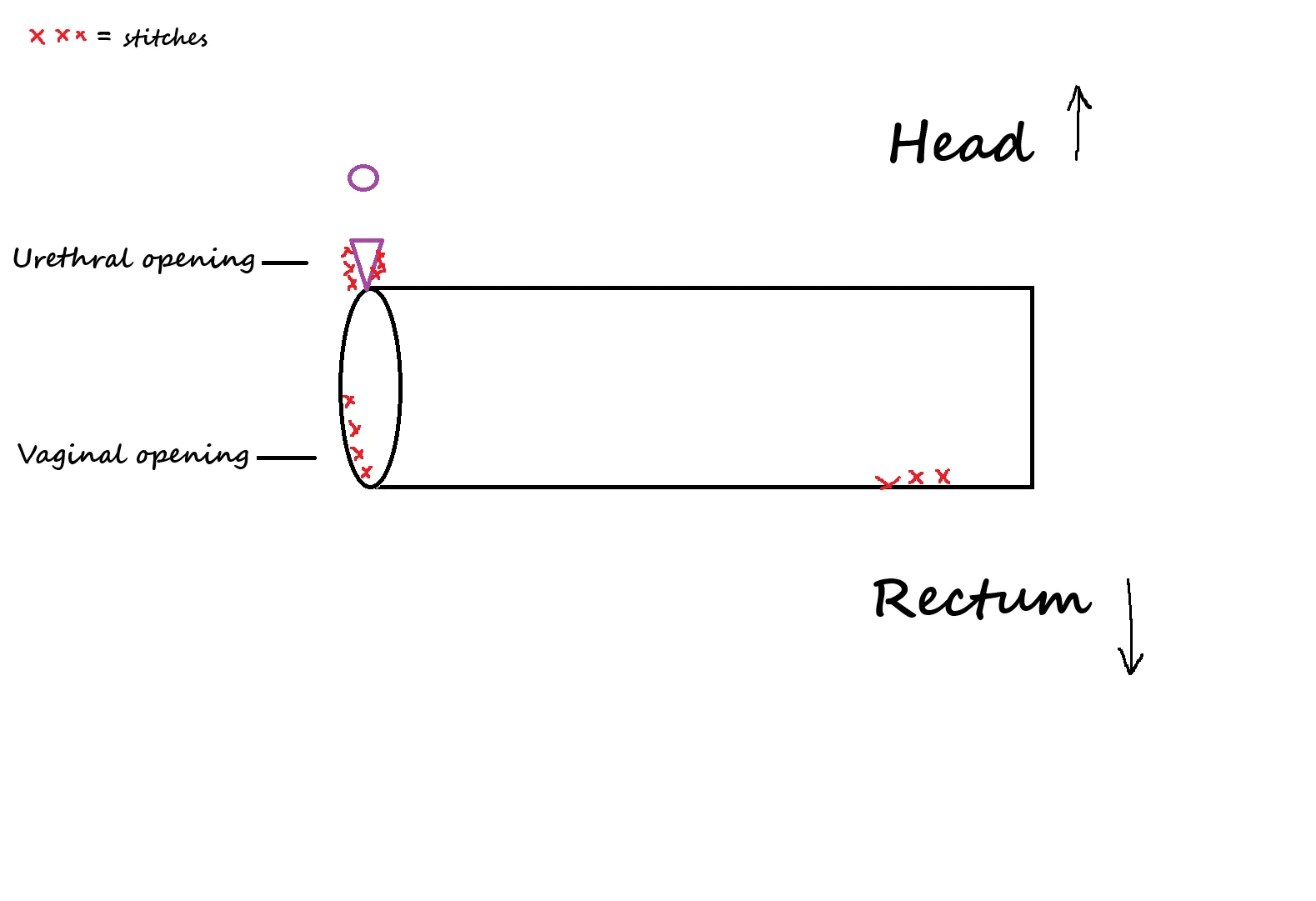
- Your diagram is perfect. That is exactly what I have done. The vagina to make the opening wider and it looks better with less vaginal webbing, and the urethra to redirect flow. The only difference is the urethra. I shaved some spongy tissue from the right side of the labia minora under it as well.
May 14, 2025
I dilated again and when I was on my last dilator I felt something pop and saw blood, it isint a huge amount so I assume a stitch somewhere has torn through.
I was dilating how I normally do but more reserved, I was nowhere near my old depth and even the girth of it feels tight and really not good which hasn’t been a problem for ages. I’m just scared I’m going to lose what I’ve spent hundreds of hours building and maintaining :( I feel scared to dilate at the moment and I don’t know what to do or what I’m doing wrong. Should I stop using my bigger dilator for a while? or will that just cause more issues because the new wounds will heal tighter? I don’t know what to do
I guess I should ask my GP if I’ve damaged stuff because I can’t see anything myself there
- Dr Hart must’ve missed this email, but it ended up being fine. I went to my GP who removed the stitches and since then I’ve slowly been getting back to my original depth (currently 09/06/2025).